The Role of the Acute Stress Response in Grief
/ Understanding Grief : Eleanor Haley
I want you to think about the worst moment of your life. When was it? What was happening? Personally, I can think of two.
- When I found out my mother had terminal cancer.
- The morning my father called me at an abnormally early hour to tell me my older brother had been in a devastating car accident. He's okay now, but at the time, and for days afterwards, we had absolutely no idea if he would live or die.
These "moments" were distinct and different, but in certain ways felt remarkably similar. Both of these instances seemed terrifying, threatening, and painful, and both resulted in an immediate physical response - increased heart rate, sick stomach, racing thoughts - as well as an emotional response.
When one perceives circumstances as extremely threatening to their emotional and physical well-being, their body is hard-wired to respond. First, note my use of the word "perceived" and remember that what one person considers threatening another may not. There are many differences in the way people react to crisis situations and perceived threat can account for some of that.
When the traumatic event occurs the person might think "I'm in shock," but the technical name for this reaction is the Acute Stress Response. The response is considered "acute" because it typically comes on quickly and subsides within minutes to hours (and sometimes days) afterwards.
Most major grief theorists made provisions for an acute stress-type response in the first step/process/task of their respective grief-models. Kubler-Ross spoke of denial; Worden discussed accepting the reality of the loss; Rando talked about acknowledging the loss; and Bowlby and Parks focused on coping with shock and numbness. Although the acute stress response varies depending on the person, situation, and level of trauma and distress associated with the death, it's important that people generally conceptualize acute stress as either part of the grief process or, how I sometimes look at it, as a precursor to grief.
Although understanding the acute stress response is useful for people facing the death of a loved one, it may also be helpful to those supporting people during times of trauma such as a grave diagnosis or death. Friends, family, nurses, chaplains, social workers, doctors and even sometimes funeral home staff might come into contact with someone still reeling from a death, especially when the death was sudden and unexpected.
Understanding acute stress provides context for what people are able to hear, process and understand. It might also prevent people from quickly labeling the situation as "grief" and responding with conventional sympathies, stories, offers of help, expressions of hope and meaning making. These are well-intentioned gestures, but it's often way too soon for the person experiencing the loss to find them helpful.
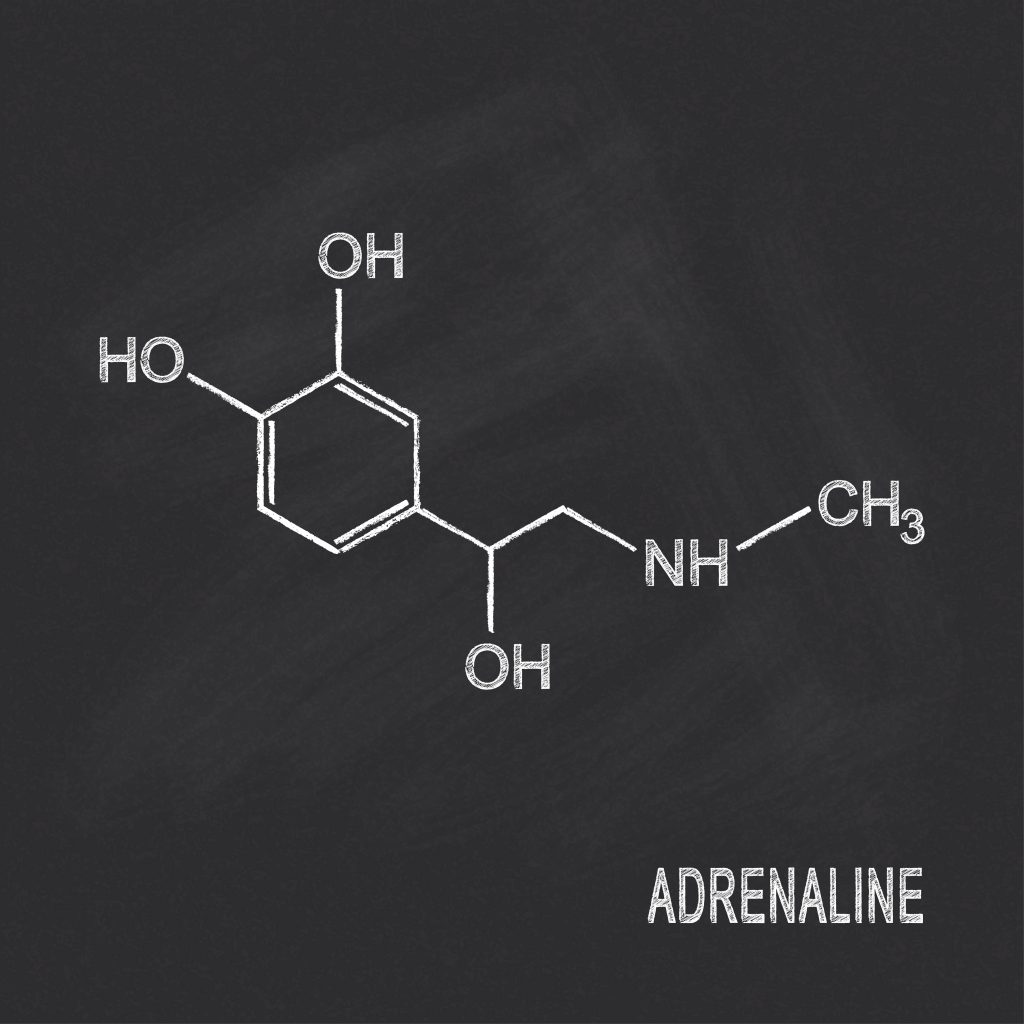
Okay so let me back up and explain how our bodies generally react to terrifying and traumatic events. The first thing a person might notice is their physical reaction to the event. This might feel like an amplified version of the sensations you feel when doing something exhilarating, thrilling, or that makes you nervous; for example last night my 5-year-old sang in front of an audience of people and afterwards she said that during the song "her body felt weird."
When one feels scared or threatened their sympathetic nervous system kicks in and triggers the 'fight or flight' response. This is a physical response that primes a person to either stay and fight the threat or run for their life. This response is seen with animals in nature and was most useful to humans in the days when they roamed the woods with lions and tigers and bears (oh my). For the purposes of this discussion, the response usually feels something like an increased heart rate, rapid breathing, muscle tension, feeling sick to the stomach, light headed, chest pains, headaches, and abdominal pains.
Additionally, acute stress can have a profound impact on our emotional and cognitive function in the following ways...
Feeling detached or numb: Although the person is physically present, they may remove themselves from the situation mentally or emotionally. This protects the person from having to face the reality of the situation and deal with the complex emotions. A person who is detached may be obviously preoccupied or distracted, however, it's possible to seem fully present intellectually and remain disconnected emotionally.
Feelings of derealization: Some may experience feelings of alienation, confusion, and unfamiliarity with their surroundings. If you consider the fact that many people are thrust into foreign environments like hospitals, police stations, funeral homes and morgues, you can see how it would be easy for someone to feel like they are living in an alternate reality.
People may also feel emotionally disconnected from those they are normally close with, as though separated by some inability to connect or communicate. Their surroundings might appear distorted and blurry or they may experience a heightened awareness and clarity.
Feelings of depersonalization: A person might feel as thought they are an outside observer of their thoughts, feelings, or body.
Dissociative Amnesia - This occurs when a person blocks out certain information associated with a stressful or traumatic event. After a traumatic event, people may say they don't remember some or all of what happened. Their memories are thought to still exist, but they have been buried deep within the person's mind and cannot be easily recalled.
Intrusive Thoughts: A person may continually re-experience the event through thoughts, dreams, memories, and flashbacks.
Avoidance: This includes avoidance of triggers and stimulus that remind the person of the traumatic event including people, conversations, or other situations; avoidance of information about the reality of the death; and avoidance of distressing memories. For more information on avoidance, please read this post.
Increased Arousal: Sleep disturbance, hyper vigilance, anxiety, problems concentrating.
Again the response will vary from person to person, but I think even a general picture of the acute stress response is illuminating. It is considered normal for this response to last anywhere from minutes to two days after a threatening event. If such overall distress lasts longer than 2 days (and up to 30 days), a person may be experiencing an Acute Stress Disorder. Of course disorders of any kind should only be diagnosed by a mental health professional using a very specific criteria.
For a more thorough discussion on supporting someone at the time of a loved one's death, head over to this post.
Subscribe to receive posts straight to your email inbox. Also, a great way to provide support to someone who's experienced the death of a loved on is by providing them with information they can read when they're ready, so check out our print grief resources.
We wrote a book!
After writing online articles for What’s Your Grief
for over a decade, we finally wrote a tangible,
real-life book!
What’s Your Grief? Lists to Help you Through Any Loss is for people experiencing any type of loss. This book discusses some of the most common grief experiences and breaks down psychological concepts to help you understand your thoughts and emotions. It also shares useful coping tools, and helps the reader reflect on their unique relationship with grief and loss.
You can find What’s Your Grief? Lists to Help you Through Any Loss wherever you buy books:





Jp July 30, 2023 at 11:22 pm
Bare with me please….My husband passed away unexpectedly 4 yrs ago. I had to find full time employment (total lifestyle change) One year later I had emergency abdominal surgery
2 weeks later, a complication, 2 weeks later another complication that took 7 months to resolve. Then a planned follow up surgery. I went back to work after being off work for 10 months. My adult daughter says if I just want to talk I should talk to a counselor, my son says if I cry I’m just thinking of myself. I went to grief counseling. Heres the problem, I have a very hard time controlling my tears at work once they start. Sometimes it’s just out of the blue…or someone says something that normally wouldn’t bother me. It’s sometimes connected to a thought process. But, overall I just have a feeling of being overwhelmed. I spoke to my doctor and I reduced the #of hours I work. That helped a lot, and I can then refrain from tears at work. I still feel pretty overwhelmed but, not all the time. Is this a normal grief thing? Or because I was so sick? Or should I look elsewhere?
Charlotte Pion March 26, 2021 at 2:16 pm
After reading Robert P. , posting, I can totally relate to his experience . I watched my husband go through 8 years of health issues .
Including open heart surgery. How very brave of you Mr P to share your thoughts. I too deal with chronic pain. Our bodies were in high gear for so long . I for one, put aside my needs to help my husband . After he passed , ( Jan. 2019) , is when my health came to the forefront.
Increased body aches ( disc degeneration in my back) insomnia, loss of self. I know some of this is due to grief . I have sought counseling etc. But what comes after grieving? Who do we finally become? Can we live with the person we have become?
Robert Podobinski March 26, 2021 at 1:55 am
wow… ok where to begin…
In May 2017 my best friend Chris was diagnosed with a very rare type of leukemia.
(I always feel I have to add this, simply saying he’s my “best friend” isn’t enough. He and I were brothers. Best friends for 26 years! A once in a life time friendship. My soul mate in a sense. Not everyone finds this in their lifetime)
I saw him go through countless chemo treatments. Each taking there toll on him. He was the most vibrant, life loving, unstoppable animal of a person. A party wasn’t a party unless he was there kind of personality. A Can do attitude with a iron will.. I saw him slowly deteriorate and fade away.
Almost a year into treatment and things seemed to get a little better. Bone marrow transplant performed. Hope was on the horizon. He seemed more himself, made jokes again, could finally have a beer with each other again.. December came with dreaded news, cancer came back and spread. Devastating .. the thoughts of hope stomped out and replaced with the consuming thoughts of my best friend, my little brother i never had , my favorite person on this earth, could die.
His choices were, ride it out, live for 6months to a year, try to find peace and eventually die.. or fly to Houston for a experimental chemo trial. He chose the later option. To continue fighting despite the very low odds he faced.
He began his trial around Christmas 2017. I video chatted with him on my bday, Jan 1st 2018. This was the last time I heard his voice. Maybe a week or less later my best friend coded. I still remember his dad calling me, telling me what happened. He died and was brought back and put into a coma.
Reality hit me.. My best friend is going to die soon.
I think that was the point where I stopped being me. Complete and total numbness slowly creeped in. Maybe it happened earlier in the year but I was so hyper focused with being there for him, his father, his girlfriend, and our friends I completely forgot about myself. I just pushed on like everything was and will be ok..
A full month in a coma now. I remember just praying he’d wake and completely forgetting he was still dying of cancer. I flew from Chicago to Houston almost every weekend to see him. In February he finally “woke”. He was paralyzed and bed riden but had brain activity. Very slowly he came to a little by little. But just as soon as a sliver of good news came in, doctors saw fit to give him a tracheotomy.. Now my best friend can’t move, can’t talk , and is fully aware of all this.
Time went on. I got really good at reading his lips. He liked when I was around for that reason. Once nurses attempted to remove the tube in his throat and blood began to shoot out every where, he looked at me and mouthed words. His dad was incorrectly translating what he was saying… He was saying the words “let me die”.. I did not translate his words.
One time his mother and I were discussing with Doctors on whats our next actions, she and I still held on to hope. Even after all this it was still in us. His dad pulled me aside in his hotel room and said “Rob, Chris isn’t making it another month.” Right when he said that I really lost hope.
March slowly came. More terrible sights and the end began to materialize. Chris wanted to die in Chicago but since being in this state he would need to be medically airlifted. I started a gofundme to help his dad. It cost 20k , we raised it in a week. For a split second the feeling of helping made me somewhat forget that I was raising money so my best friend can die in his hometown.
He flew back to Chicago.
After several weeks of his health fading, the doctor came in and said to us, he thinks its time. The doctor asked Chris if he wanted to pass on. Chris looked around and calmly replied a phrase hes said hundreds if not thousands of times in his life. The perfect words that encapsulated his larger than life energy. His always down for adventure personality. Words that broke me and words that still hold me together..
My bestfriends last words:
“Lets do it!”
Chris died April 3rd, 2018… he was 29.
I sat there holding his hand while they gave him morphine , he drifted away to sleep. I saw his last breaths and then he was gone. Nurses turned off the Machines and left the room. At this point I was already stone cold numb. Other people were crying, all I could muster up was a single tear and some trouble breathing for minute. I can still feel the eerie silence of the room. That silence has stayed with me ever since.
I left the hospital and drove home. I don’t remember driving at all. But I remember everything else.
After less than a year of being diagnosed Chris’s nightmare ended.
Mine was just beginning.
The second after he died I literally felt my emotional connection with the world turn off. I don’t know how else to describe it. The world no longer spoke to me as it once did. I became a stranger inside myself.
Love, happiness , joy, affection were no longer something I felt. They were only words I seemingly lost the definition to. I died that day too, but i was left behind.
In the months following his passing, ofcorse I knew I was depressed. Who wouldn’t be?! But at the same time I didn’t know what that meant. I never knew such a feeling before. I think I’ve had some minor depression issues stemming from childhood stuff but nothing close to this.
“Depressed” a small word with a earth shattering sized spectrum.
I’m depressed the bulls have been a terrible basketball team for 20 years. I’m depressed when one of my dogs passes. I’m depressed I started going bald at 21.
If thats all being depressed, then what is it that I feel now??
Its hard to describe “being depressed” to friends and loved ones. Its something I’ve struggled to do so up until this moment as I write this almost 3 years later. Not only the feeling one feels when in its deep dark fog, but the very ability to explain goes away. Caring goes away. The will to do anything goes away.
The symptoms them selves isolates you. It makes you not want to share. Ive found It simply makes you want to be ( for a lack of better words) more depressed!
Ofcorse I knew i had to grieve. But I didn’t know what that meant. I still don’t. My emotional systems still don’t work.. I didn’t feel like grieving. I was just numb. I didn’t know how to get “help”.. I prayed and prayed that I would get through it. Wake up some day and be me again… it never happened. Before I knew it, I became lost.. never to find myself again.
At the time I was in a relationship with the love of my life for 8 amazing years.
(A little about me first, I’ve always loved easily. Gave the person im with everything I had. Selfless and sensitive. Heart on my sleeves kinda guy.) Up until this point my gf was the end all be all and I was completely content. I cant stress this fact enough. I loved her wholeheartedly. Then Chris died.. the person I was died. The love that I felt waking up in the morning that got me through another work week was gone. I stayed in the relationship for 2 years feeling this depression. I spent day after day, week after week crying in my work car. I felt so miserable about not being in love and also hating myself for feeling this way. I thought about suicide from time to time. Thinking it was a better option rather than actually breaking up. I was in a very bad state.
My girlfriend was a almost full time student and worked opposite times than me. Which really made me feel even more alone and isolated.. Not her fault at all but caused its damage. She also was going through her own stuff.. she was depressed too, which also pushed me away.. I now am able to see what led me to believe that we just simply grew apart. Thats what I told myself then, because I was just trying to make sense of all these terrible feelings I’ve had for so long. I just wasn’t able to see past the depression I was in.. I put the blame of my pain and sadness on my failed relationship. But I know now that wasn’t the case.
So after 2 years of fighting this, I gave up. I was so detached emotionally, and mentally. So desperate to feel something again. I was so sick and tired of being unhappy I broke up with the person I thought I’d be with forever. This haunts me every day. I know when I was in charge of my mind and wasn’t depressed she was the one i chose to love.
Lets back track. This is extremely important.
Starting at the begining of the same year of Chris’s diagnosis, I began having side pains in my lower left abdominal area. It continued throughout the ordeal with Chris and long after.
During these 4 years I’ve also had extreme bouts of insomnia.
I havnt slept more than 5 hours in a night in over a year. And that’s with taking a cocktail of sleep aides. There has been extremely long durations where I’ve gone weeks with out sleep.
The inability to relax due to having chronic pain ,extreme anxiety of not knowing what is wrong with my side combined with severe insomnia for 4 years now is enough to cause someone to go crazy in itself…I’ve learned having chronic pain can also lead to a entire slew of mental health issues.
The mental strain of this alone I believe has been even more damaging than Chris’s passing. Its honestly hard to say at this point. I honestly don’t remember what its like to be healthy and not it pain. I havnt been able to enjoy life for over 4 years now. Every aspect of life I am in pain.
..i don’t know why I didn’t seek help back when I first felt depressed. Its easy to say that now 3 years later…it just seemed I couldn’t. However 3 years of depression research and alot of self reflection have really made me understand what happened to me.. i know now ive been severely depressed for a long time.
Everything I described has taken its toll on me mentally and physically. This entire ordeal has caused me severe mental problems. The combination of losing my best friend, losing my love for being alive, losing the person I loved , losing my health , losing the ability to simply relax and being able to sleep has convinced myself there is no hope. I truly think I’m slowly dying..and ill be honest
I don’t want to be alive either. No1 knows what I’ve dealt with for all this time. I have no escape. No one on earth should go through this.
I know depression makes you crazy. Having chronic pain for long periods of time can also lead to mental illness. Lack of sleep is the most dangerous and I have all 3…
Im feeling like by body is giving up. I don’t feel like I have it in me to continue like this anymore.
I will go back to Dr soon.
Ill tell him all this. See where that takes me. But the hope of being healthy and healed some day seem impossible.
I’ve never put all of my pain in words before.. this article made me think of alot of things and it gave me energy to write.
Mary March 25, 2021 at 5:50 pm
Hi this was good to read but I have lost 3 of my children my three youngest my son took his own life at just 16 just a year ago one lived 4 weeks one child lived 8 days but my son who took his own life was such a shock to my life it is hard to explain it hit me that bad I did not want to live I tryed takeing my own life cause I could not cope I’m still feeling it very bad I think im still in shock my son never showed any sign of depression which made the hole thing harder to deal with I dont no if I will ever get over the loss of him the pain has got so much worse
Sabine Horner January 31, 2021 at 10:12 am
Based on what I have learned from research into our stress response and from my personal experience with grief, distress lasting longer than 2 days is absolutely normal in grief (and not an Acute Stress Disorder). It is called chronic stress. It doesn’t need a mental health professional or GP. Neither do people need medication. They need proper stress management through deep breathing, meditation, yoga, Tai Chi etc. Anything that stimulates the vagus nerve and puts us back into rest-and-digest-mode. Digestive issues caused by this chronic stress are very common in grief and the cause of many nutrient deficiencies which, if not addressed, can lead to serious health issues further down the line. Grief is not something you get over in two days. Neither is the shock and numbness of seeing your loved one die in front of your very eyes.
Isabelle Siegel January 31, 2021 at 10:21 am
Hi, Sabine. Thank you for taking the time to comment and to share your perspective. You’re right– It’s totally normal and okay for distress to last for longer than two days, especially in the context of grief. That being said, sometimes it IS helpful to seek out the support of a mental health (or other) professional.
Sabine Horner January 31, 2021 at 12:48 pm
Hi Isabelle,
There is always a role for mental health coaches and bereavement support workers in grief. I just wanted to make sure grieving people don’t start to think that there is something wrong with them because they are numb or in shock for longer than 30 days. And it is important for mental health coaches and bereavement support workers to be aware of this chronic stress causing digestive issues and therefore nutrient deficiencies which then cause or contribute to depression, anxiety and other mental health issues. You will be able to read my guest blog on this topic for Full Circle Funerals on their website shortly. My next episode for Food Friday on Inspire Radio will also cover the many contributing factors to anxiety issues.
Tiffany March 8, 2020 at 10:58 am
Are thoughts of wanting to be with your loved one, normal? So lonely even with people around me. It’s been five months since both parents passed. I feel like I want to be near them and feel safe and loved by them again. I have a beautiful life and do not want to go to heaven just yet. I just miss them so much.
Rita Dey June 24, 2019 at 2:06 am
I lost my husband 6 months ago. It’s only the last couple of mo ths that the reality of it has set in and I’m very teary although not crying a lot.
I’m finding it really hard to deal with anything stressful. If anything is difficult to do I just dont want to do it at all.
My stress level can go from 1 to 10 in 2 seconds. I’m not usually like this is it normal?
Catherine Brown March 19, 2019 at 9:14 am
My grandson was born with many health issues, only 6 months cognitive. In August, after being in and out of the hospital since March, we were told no more could be done for him. His 14 year old body couldn’t digest his feed. On December 10th, he past due to starvation. Since this wasn’t hard enough for me knowing I was going to lose him, I came home on November 13th, from being with him, to find my husband in the tub. He had drowned due to reasons that lawyers are involved. Since all of this, I am dealing with complicated grief and acute anxiety along with depression. It’s been four months and I still feel like I’m dying. I’m on medications and seeing a psychotherapist. I do not want to go out or talk to people but don’t want to be alone. My daughter has been with me.
I’m praying to get over the most biggest hurdle in my life.
Jennifer Hatton February 11, 2019 at 5:19 pm
My husband of 30 years died after a four month illness. His 1st anniversary is approaching and I am definetly suffering with anxiety. Every little task I have to do feels like a mountain. Can’t make a decision about anything. My sleeping and eating is all over the place. When I’m in company I feel so detached. When I start to cry, I stop myself. Don’t know if this is because I promised him I’d be happy or afraid I won’t stop if I start.
SJ January 8, 2020 at 10:35 am
Dear Jennifer,
I’m sorry to hear of your loss, and your experience with grief so far. Please know that you are not alone in feeling this way approaching the anniversary of your loss… and now approaching another… it is an experience many have, approaching milestones like birthdays, actually all the ‘firsts’ of that initial 12months… especially the first year marking the loss of your loved one, but also in subsequent years. The anxiousness and apprehension is natural considering the significance of the anniversary and what it means to you emotionally. Humans are by nature are ‘meaning markers’, we create rituals around emotionally significant events because it helps us to process, understand and move through these events and time. This word ‘significance’ can help during this time, the lead up and the ‘during’ of the anniversary day, if we use it to ourselves in our internal self-talk, when you feel the anxiety rising, perhaps a sense of pending revisiting of the grief, talk soothingly to yourself… ‘yes, this is a very significant anniversary to me, to me emotionally… and this is natural that I am feeling heightened emotions around this time’. This sense of significance honours the depth of your love and respect for your loved one. One way to release this anxiousness is through shedding tears, letting the body feel physically what you feel emotionally. It is also very natural to worry you won’t be able to stop crying. Prior to release, the pressure feels immense, but nature is kind, grief rises and falls in waves – you can trust nature in this fact – once you are feeling overcome with emotion, really sobbing, nature will let you feel only a limited amount of pain.. then it will retreat. And provide time for reprieve. Trust this cycle. It will help you to *allow* your feelings to come up, to feel them and yet not feel overwhelmed by them in an ongoing way.
In practical ways, support yourself by reaching out to someone close and asking them to be with you for that day, or part of that day, or to do a small ritual that day like make a flower arrangement or even walk through a particular park or place. Confide in them that you don’t know if you will be saddened on the day, or anxious, or experiencing fond memories, likely all three, and ask for their kindness and support through these varying emotions. If you aren’t sure who to reach out to like this, talk kindly to yourself… ‘whether I am saddened or full of fond memories, both are valid for the depth of feelings I had and still have for him, I will let myself grieve and honour in the emotions I feel. Movies and the characters in them, can be great company if a friend or family can’t be present. They can also provide a comforting arc to experience your emotions within.
In my experience of losing a loved one, a close family member was the bereaved fiancé and in years since (4years) that day is spent together just for company sake, and because many friends don’t understand that 1year or 2 years doesn’t feel like years actually.. emotionally time passes differently. My thoughts are with you.
Diana September 1, 2020 at 2:22 am
Thank you for comment. My dad passed away a month ago and I’ve been flooded with panic and anxiety since. Your comment gave me direction and made me feel better. I like the part where you said grief comes in “waves”, this makes it feel more manageable.
Marjory Copeland October 23, 2018 at 6:33 pm
I lost my daughter to cancer 3 years ago and it feels like it happened yesterday .
Is there something I can do to work through the grief ?
Linda March 11, 2018 at 5:07 pm
My son 34 years old lost his partner to a heart attack age 31Jan 6 2018 he is almost totally blind he spent the night at A&E last wed chest pain breathless racing pulse and raised blood pressure and had been drinking he was discharged to gp who gave him valium and was already on citalopram he has since taken to bed with limited contact and
Linda March 11, 2018 at 5:07 pm
My son 34 years old lost his partner to a heart attack age 31Jan 6 2018 he is almost totally blind he spent the night at A&E last wed chest pain breathless racing pulse and raised blood pressure and had been drinking he was discharged to gp who gave him valium and was already on citalopram he has since taken to bed with limited contact and
Jacinda Padilla June 21, 2017 at 11:47 am
I am taking this course because I would like to help people in my community that are grieving. I work for a community based organization. This particularly hits home to me because personally I am grieving. I lost my husband almost 10 months ago. I have definitely felt things like sleep disturbance, derealization, and avoidance.
Gretchen Greeley Waters March 21, 2015 at 8:19 pm
Although my husband had terminal cancer, I expected him to live longer than 3 months after the diagnosis. His death was sudden and very unexpected. I initially was relieved as he was suffering so, but then the reality of it all kicked in. As I suffer from both depression and anxiety, I isolated myself from the world. Since his death I have lost 60 lbs…..I am happy at the weight I am now at and have been to see my physician for a complete physical – coming out with a clean bill of health. I see both a psychiatrist and a therapist (bi-weekly) to help me cope with my husband’s death. As with grieving, I take it one day at a time just to survive. I am slowly – slowly – making strides and am now doing volunteer work to honor my husband’s legacy.
Eleanor March 23, 2015 at 9:09 am
Gretchen,
I am so sorry about everything that you are your husband went through. I understand it has been a struggle for you, but I do have to say it sounds like you are being really proactive and are doing as well as possible. So congratulations on being able to get out of bed and take it one day at a time 🙂 I guess that’s the best many of us can hope for!! I’m sorry about the death of your husband, I am sure he is dearly missed.
Eleanor
Laura March 18, 2015 at 6:49 pm
When my son died suddenly three years ago, I had “Increased Arousal: Sleep disturbance, hyper vigilance, anxiety, problems concentrating” for a full two years afterward, not two to thirty days. I saw a therapist and a psychiatrist and neither one brought up the fact that this was abnormal, but I did receive some good support. I took three months of that time off, which was all I could afford. I was walking zombie the rest of the time. My boss marked me down on my evaluation and also said I missed too much time. I wanted to scream at him, “Do you even realize it’s a miracle every day for me to just show up?” I didn’t want to talk to anyone either for a while – it was too painful. I broke off some friendships because I just couldn’t maintain the contact. I gained twenty pounds. Only in the last year have I started to feel like a person again. Hugs to all of us going through horrible experiences – the world has a hard time understanding us.
Daisy March 17, 2015 at 7:50 pm
I was already living with Complex PTSD when my husband of 34 years died last year.
During his 7 month illness, and because I’m also an introvert, I found it intolerable to have to manage people who wanted updates on how he was going. Ultimately I just tried to avoid stress triggers as much as I could. For my own sanity, I just ignored all but my closest friends and family.
After his death, it all intensified, and my usual stress management of walking became really difficult as I kept meeting people who wanted to know how I was doing. After talking about with my therapist, we decided avoidance was the best option for me, and I took to getting up very early and walking then. If I did meet anyone I knew, I pretended to be talking on my mobile (cell) phone until I passed them, so I wouldn’t be expected to stop.
8 months later and I feel much better and on a good day able to talk to people again, although I usually say after the initial “I doing ok, good days, bad days etc” that I don’t want to talk about it. I still not ready to go there and I still experience very a strong stress response talking about T’s illness and death.
Now, it’s only very rarely that I need to pretend to be on the phone.
Pam March 17, 2015 at 5:06 pm
What perfect timing!!! this was a huge help for a couple of clients of mine. Thank you so much. I always enjoy your posts.
sandy March 17, 2015 at 3:35 pm
I experienced amnesia after henrys death. I still dont remember details about the funeral or wake. For 3 or 4 days after i was in shock, spoke slowly, they thought i had to go in a facility for shock( i havr a history of depression). I was ok after a while. But i do avoid certain places we used to go, just cant face going there without henry. Hopefully in time i can.
Marty Tousley (@GriefHealing) March 17, 2015 at 1:13 pm
This information is important, Eleanor, and I thank you for writing this. As a hospice bereavement counselor, I’d sometimes get a referral from a member of our hospice team immediately following a death, out of genuine concern for a family member who seemed to be “hysterical” or “falling apart” ~ when what was really happening was the person’s initial reaction to the loss, which can look and sound quite “crazy” to the observer. So often this is simply (as you say) an acute stress response. That is why in most instances rather than right away, we’d prefer to contact a family two or three weeks following the death, thereby giving the bereaved sufficient time for things to settle down a bit before offering grief support.